Lung Cancer: The Most Common and Deadliest Cancer Worldwide (2026 Guide)
Lung cancer is the uncontrolled growth of abnormal cells in the lungs, forming tumors that can spread (metastasize) to other parts of the body. It is the most common cancer worldwide and the leading cause of cancer-related deaths, responsible for more fatalities than breast, colorectal, and prostate cancers combined. According to the latest GLOBOCAN estimates (2022, with projections stable into 2026), there are approximately 2.48 million new cases and 1.82 million deaths annually. In many countries, including Turkey, it ranks high among male and female cancers, with smoking as the primary driver.
When caught early (localized stage), 5-year survival rates can exceed 60-67% for non-small cell types; overall, however, the global 5-year survival is around 25% due to late diagnosis in most cases.
Types of Lung Cancer
- Non-Small Cell Lung Cancer (NSCLC) → ~85% of cases; slower-growing. Subtypes: adenocarcinoma (most common, especially in non-smokers/women), squamous cell carcinoma, large cell carcinoma.
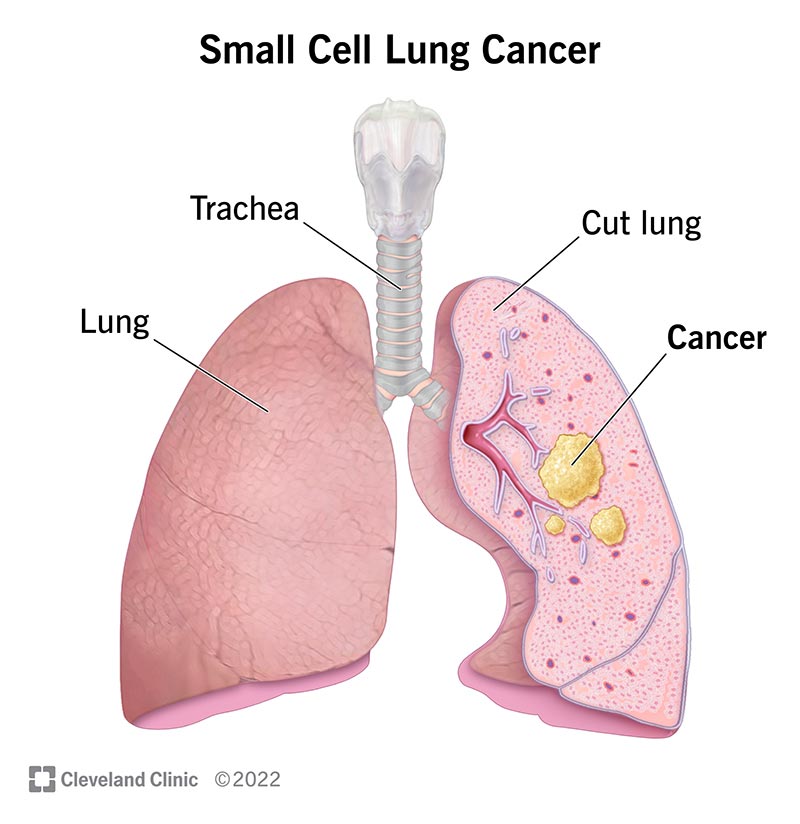
- Small Cell Lung Cancer (SCLC) → ~15%; aggressive, fast-spreading, strongly linked to smoking.
Symptoms
Early lung cancer often has no symptoms; that's why screening is crucial for high-risk individuals. Common signs when advanced:
- Persistent cough or worsening of chronic cough
- Coughing up blood (hemoptysis)
- Shortness of breath, wheezing, or chest pain
- Hoarseness, unexplained weight loss, fatigue
- Recurrent infections (pneumonia/bronchitis)
- Bone pain, headaches, or neurological symptoms (if metastasized)
Any persistent respiratory change warrants immediate medical attention!
Risk Factors
- Tobacco smoking → Accounts for ~85% of cases; risk increases with duration and intensity.
- Second-hand smoke exposure
- Radon gas, asbestos, air pollution (especially PM2.5 linked to adenocarcinoma rise)
- Family history, previous lung diseases (COPD), occupational exposures (diesel exhaust, etc.)
- Note: Increasing cases in never-smokers, particularly adenocarcinoma in women/younger people due to pollution/genetics.
Diagnosis Methods (2026 Updates)
- Low-dose CT screening → Recommended for high-risk (heavy smokers 50-80 years); reduces mortality by ~20%.
- Chest X-ray, CT/MRI/PET scans for staging
- Bronchoscopy or needle biopsy for tissue confirmation
- Molecular testing (NGS) → Essential for NSCLC to identify actionable mutations (EGFR, ALK, ROS1, BRAF, etc.)
- PD-L1 testing for immunotherapy eligibility
NCCN/ESMO 2026 guidelines emphasize broad biomarker profiling early.
Stages and Survival
- Stage I (localized): Tumor small/confined to lung → 5-year survival ~60-67% (NSCLC); surgery often curative.
- Stage II (regional): Spread to nearby nodes → ~35-40%
- Stage III (locally advanced): Larger/local spread → ~20-30%
- Stage IV (metastatic): Distant spread (brain, bones, liver) → ~5-10%; managed as chronic with modern therapies.
SCLC uses limited/extensive staging; extensive has poorer prognosis (~2-4% 5-year survival).
Treatment Approaches (2026 Current Standards)
Treatment is personalized based on type, stage, biomarkers, and patient health (multidisciplinary team):
- Surgery → Lobectomy or segmentectomy for early NSCLC (curative intent).
- Radiation → Stereotactic body radiotherapy (SBRT) for inoperable early-stage; chemoradiation for stage III.
- Chemotherapy → Platinum-based (e.g., carboplatin/pemetrexed) for advanced; neoadjuvant/adjuvant.
- Targeted therapies → For driver mutations: osimertinib (EGFR), alectinib (ALK), etc.; dramatically improve survival.
- Immunotherapy → PD-1/PD-L1 inhibitors (pembrolizumab, nivolumab) alone or with chemo; first-line for many advanced cases.
- Newer options → Antibody-drug conjugates (e.g., datopotamab deruxtecan), combination regimens.
With advances, many stage IV patients live years with good quality of life; lung cancer is increasingly "chronic manageable" for some.
Prevention and Early Detection Tips
- Quit smoking immediately → Biggest impact; risk drops significantly over time.
- Avoid second-hand smoke, test home for radon.
- High-risk individuals: Annual low-dose CT screening (50-80 years, 20+ pack-year history).
- Healthy lifestyle: Exercise, balanced diet, limit pollution exposure.
Early detection saves lives! If you're at risk or have symptoms, consult a pulmonologist or oncologist without delay.
📚 Связанные заболевания
Узнайте больше о связанных онкологических заболеваниях:
Yorumlar (0)
Henüz yorum yapılmamış. İlk yorumu siz yapın!